Demands for accessibility and image quality are key drivers for transducer advancement
By Elaine Sanchez Wilson
This month, 24×7 Magazine took a look at the ultrasound transducer market and sought insight from industry experts who commented on major factors driving innovation for this critical component. Topics ranged from opinions on up-and-coming applications, to recommendations for proper handling and storage.
Roundtable participants included Said Bolorforosh, president and head of ultrasound at Malvern, Pa.-based Siemens Healthineers; Dave Dallaire, vice president of sales and marketing at Longmont, Colo.-based Acertara; Diku Mandavia, MD, FACEP, FRCPC, senior vice president and chief medical officer for Fujifilm SonoSite and Fujifilm Medical Systems USA Inc. in Bothell, Wash.; and Matt Tomory, head of strategic advancement at Whippany, N.J.-based Bayer Multi Vendor Service.
24×7 Magazine: What are the top trends in the ultrasound market that your company is monitoring, and how will they influence the design/development of ultrasound transducers?
Said Bolorforosh: I see three trends happening, which is focusing on the patient, the payer, and the provider. And those are basically the three drivers for our environment.
When we first look at the patients, for example, there is an increase in obesity trends, globally. That leads to a number of things: One is seeing what types of technologies we can bring into the market to help manage, monitor, and treat various diseases around obesity, such as cardiovascular disease or diabetes.
If the patients are too big to scan—[making it] difficult to obtain good diagnostic image quality, then we must make sure that we design our ultrasound solutions to produce good image quality in these difficult-to-scan patients.
Now when it comes to the payers and the hospital administrators, their requirements are different. They look at, for example, uptime of the equipment: Is the equipment up running 24 hours a day, seven days a week, without any instructions or failures?
They also look at the cost of the equipment: Are they going to finance it? Is it cost competitive? They look at consultation, and help with fleet management of the various ultrasound machines that they have in their hospitals. After all, some of our customers have a few hundred Siemens ultrasound machines in their hospitals and clinics. And they look at us to help them to decide how to best utilize those assets.
Dave Dallaire: The top two trends we watch very closely are:
• Higher levels of integration of beamforming and image-processing technologies into the transducer and away from the system front-end
• The continued diffusion of diagnostic ultrasound into non-traditional markets, such as home healthcare
These two trends have been driven by where the broader technological world has been heading since 2008—smart technology empowering the “Internet of Things.” In many respects, we’re already there. For example, the Vancouver, B.C.-based company Clarius recently introduced an ultrasound probe that wirelessly connects to a smartphone to display and process the B-mode image, as well as color-flow Doppler.
These technology trends, coupled with deep learning and artificial intelligence, will allow clinical personnel who are not ultrasound experts to use diagnostic ultrasound in underserved and remote parts of the world.
Diku Mandavia: The first trend is new advancements making ultrasound accessible. Due to patient concerns over the radiation dose associated with CT scans and new advancements in ultrasound technology, ultrasound has become a vital modality and plays a ubiquitous role in hospitals across departments. Due to the advanced imaging quality and focus on patient safety, my prediction is that all physicians will utilize highly mobile ultrasound in the future.
No.2 is the focus on patient outcomes. With an aging population and an increase in chronic conditions and unhealthy lifestyles troubling the American population, a focus on patient-centered care is critical to addressing these health risks. Today’s healthcare ecosystem has a focus on providing positive health outcomes, comfort, and personalized attention for each patient.
In addition, as the healthcare system moves from a fee-for-service to a value-based model of care, offering financial incentives for quality of care rather than the quantity of services provided, Fujifilm will continue to innovate to help our customers with operational efficiency for hospitals, best practices, prevention of diseases, and dedication to improving health outcomes.
Matt Tomory: Ultrasound is a fairly mature technology when it comes to systems, so we are seeing incremental progress in probe technology designed to improve image quality. One of these advancements is matrix array technology. With traditional transducer arrays, individual elements are arranged in a row with 192 or more elements.
With matrix arrays, there are rows and columns of elements and element counts in the thousands. This allows for improved image quality, but it also increases the cost of purchase and is exponentially more complex to repair. Ultrasound transducers may be involved more in image processing than in the past, as well.
Some transducers perform much of the beamforming that took multiple circuit boards a generation ago or—back when I started with the Acuson 128 in 1986—dozens of boards.
24×7: Which clinical area(s) do you expect to see the most growth in the coming years, with regard to ultrasound use? And what technological advancements have been made to ultrasound transducers used in this specialty?
Tomory: The point-of-care ultrasound market continues to grow with no foreseeable end in sight. Systems have been getting smaller and more capable than ever before and, as mentioned previously, the transducer may be doing more of the image processing. We are beginning to see ultrasound apps with the probe performing all aspects of image formation and processing.
Mandavia: Ultrasound-guided procedures in regional anesthesiology, musculoskeletal ultrasound, and vascular access procedures are gaining wide acceptance as standard of practice. Ultrasound guidance provides greater accuracy in identifying target structures so procedures may be performed more quickly and efficiently. This application of ultrasound addresses both the hospital’s need to perform procedures safely and to improve the quality of care they provide.
Continued research and development has focused on improving image quality and transducer efficiency. Fujifilm SonoSite, for instance, has developed DirectClear technology that combines several new design features for significant performance improvement including: matching layer technology to enhance bandwidth, resulting in increased detail resolution of fine structures; single crystal technology to improve transducer efficiency; and reflective layer technology to improve signal penetration.
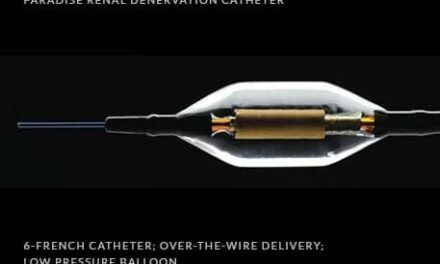
Dallaire: We are seeing a convergence in many clinical areas related to ultrasound image-guided treatment, such as with prostate cancer or uterine fibroids—essentially coupling diagnostic ultrasound with focused ultrasound and its various derivatives, such as highly focused ultrasound.
Continuing advancements in highly sensitive transducer crystal materials, 2D matrix arrays and volumetric imaging, as well as the broader application of novel array materials, such as capacitive micro machined ultrasound transducers, will all be essential to the combination of ultrasound diagnosis with ultrasound treatment.
Bolorforosh: There are a few areas where we definitely see growth. Some of it is in the core markets: radiology and echocardiology. Those are the more traditional segments that grow at a steady rate, and we must make sure that we cater to that part of the customer demographic.
The other segment is the emerging applications—the new ones that are growing much faster and are basically expanding ultrasound utilization to newer clinical care areas, such as point-of-care ultrasound and interventional cardiology.
The point of care covers multiple specialties, such as sports medicine, regional anesthesiology for pain management, critical care, emergency medicine, and ambulatory care. It is basically bringing ultrasound into the bedside of different specialties, and helping them with the diagnoses, treatment, or guidance of the procedures. Also, with interventional cardiology, many cardiac procedures are becoming minimally invasive, and there are two modalities that primarily support it: x-ray and ultrasound.
The third area is basically trying to extract more information out of the ultrasound image. Shearwave elastography is where you actually get information about the tissue stiffness, which is really important when it comes to early diagnosis and characterization of lesions. And the last area is contrast-enhanced ultrasound, which has a similar application idea, where we are trying to visualize microvascularization.
24×7: What special considerations must HTM professionals have in the maintenance and repair of the newest generation of ultrasound probes?
Dallaire: The gating issue with repairing any technologically intensive medical device is the ability to objectively test the device, diagnose what the failure is, and then post-repair test again to ensure the repair was effective.
Bolorforosh: We encourage our customers to follow the manufacturer-recommended care and handling instructions for the transducers. Some of these probes contain tremendous amount of highly miniaturized electronics, which makes them fragile. It’s a little bit like your cell phone or your camera—you have to make sure that you handle it with care.
The second part of transducer care relates to disinfecting, sterilizing, and cleaning the probes. Some of these cleaning chemicals are quite harsh. And, as a result, any extended exposure of the probes to these chemicals can cause damage to them. We recommend our users follow the manufacturer’s instructions to maximize the life of their probes.
Tomory: Ultrasound transducers are extremely sophisticated medical devices and must be viewed as such when repairing. The science, technology, equipment, knowledge, experience, and processes required to perform a repair to ensure OEM form, fit, and function cannot be overstated.
Repair facilities must be able to demonstrate they are ensuring all acoustic characteristics are within what the OEM intended the probe to do, as well as ensure biocompatibility, compatibility with the OEM-recommended cleaning and disinfecting solutions for materials, and safety.
Mandavia: High-level disinfection of the transducers is a requirement after use. Cleaning and disinfecting solutions are tested for each transducer. For ongoing maintenance of the transducers, it is critical to use an approved cleaning and disinfection solution so the transducer-housing material is not damaged.
24×7: Please share some other best practices for extending the longevity of ultrasound transducers.
Tomory: First, you need to follow the OEM care and handling instructions. Second, inspect probes regularly for any damage to the lens, cable, connector, or array. A minor defect found early is a much less expensive repair than a catastrophic failure. This is especially critical with TEE probes, where an electrical safety test is also recommended (or mandated if Intersocietal Accreditation Commission-accredited). This test is for patient safety, but it can also identify a breach in the probe, which may allow fluid to intrude—[thus] rapidly degrading a probe.
Dallaire: The majority of defective probes we see from hospitals generally have been damaged because of improper use (e.g., not using a bite-guard with a TEE probe), improper cleaning methods or chemicals used, and improper storage/transportation. Guidance that addresses all the issues above is provided in the OEM probe manuals, and if followed consistently will lead to an optimal lifecycle for any given probe.
Also, it’s very important to have an evidence-based quality assurance program in place for the probes that includes routine testing and evaluation. This will allow any defects to be discovered earlier while the probe can still be economically and safely repaired.
Mandavia: A leading cause of damage to the transducers is the caustic nature of high-level cleaning and disinfection solutions. The use of approved cleaning and disinfection solutions will ensure the longevity of the ultrasound transducer.
Bolorforosh: Also, make sure the recommended chemicals are used. And when it comes to repairing the probes, contact the original equipment manufacturer. They use the original manufacturer parts and components, and they can test to the same original device quality.
24×7: For potential customers who are searching the marketplace for their ultrasound of choice, what advice can you give to help them with their ultimate purchase decision?
Mandavia: The first step is to evaluate the needs of the specific imaging facility or hospital. In addition, reducing expenses and maximizing space are key factors. Point-of-care ultrasound machines may provide the most value. As hand-carried, point-of-care systems, they are much smaller than conventional cart-based systems.
Moreover, the accessibility and mobility characteristics of point-of-care ultrasound machines make them an asset for facilities catering to bedside exams and emergency physicians, providing increased speed, patient safety, and clinician efficiency improvements.
Bolorforosh: If you look at the trends that are changing within the healthcare industry, in terms of consolidation, industrialization, and also managed health, which basically drives economic efficiency, how do we translate these into what should the customers look for when it comes to buying diagnostic equipment?
Obviously, they should make certain that the performance and functionality features meet their requirements. They should also look beyond just the equipment—and look for partners who can provide services such as consultation, education, and training.
Education and training are becoming more and more important. As the equipment is becoming increasingly sophisticated, and as the tools of the procedures are becoming more complex, we easily see the need for five to six full days of training to be able to fully utilize all the functionalities and capabilities of an ultrasound machine. Also, the manufacturer must have the infrastructure and the training materials in place to be able to meet the educational needs of the customers.
Dallaire: Don’t “over-buy”—purchase the ultrasound system and probes that best match the clinical environment and clinical applications for which it will be used. In 2017, just because an ultrasound system may be more expensive, it does not mean that it produces better clinical information than less-expensive devices. You gotta love Moore’s law.
Tomory: Fortunately, clinical engineering/HTM departments are becoming more involved in purchasing decisions of new equipment. The market is filled with excellent equipment from many OEMs, but I recommend you choose based on several key points including the availability of manuals, diagnostics and training, and market share. [After all,] there is a direct correlation between market share and the ability to support system and probe repairs on units outside of the OEM.
Elaine Sanchez Wilson is associate editor of 24×7 Magazine. For more information, contact associate editor Elaine Sanchez Wilson at [email protected].