Biomeds at Children’s Medical Center Dallas were a vital part of surgery to separate conjoined twins Mohamed and Ahmed Ibrahim. Join Ron Greenwalt as he takes us hour-by-hour through this day in the life.

Throughout the night, the delicate clamp, snip, and seal process continued. The much-anticipated bleeding problems associated with cutting the largest of the veins did not occur, and, around 11:00 am, the surgeons were satisfied that they had taken care of the final vessels connecting the boys. This was it!
When the bed was ready, the surgeons began pulling ever so gently in opposite directions. As the operating-room floor began to be visible between the boys and the last few vessels were snipped and sealed, the boys were finally separate. “We have two boys!” was the call from someone in the room.
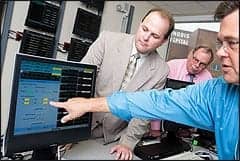
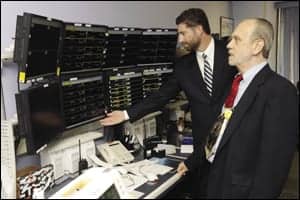
Biomed Joins the Team
The biomedical engineering department was asked to get involved in the very complicated surgical procedure to separate 2-year-old craniopagus twins Ahmed and Mohamed Ibrahim only a couple of weeks prior to the surgery. (Craniopagus means joined at the skull. The rarest form of conjoined twinning, it occurs in about 2% of cases or once in 2.5 million deliveries—Ed.) At first, the surgery was expected to take anywhere from 30 to 60 hours. As the day grew closer, the estimated time grew to as much as 96 hours. It was not going to be a normal day in the life of a biomed at Children’s Medical Center Dallas.
Olin Dillard, Sr, BMET and team leader for perioperative services, and Andrea Brainard, a member of Dillard’s team, were responsible for biomed operations and logistics. Dillard determined that we would need to know exactly what equipment was going to be in the room during the surgery and then multiply most of it by 2. This would give us a base to start the calculations for sorting out one of our biggest concerns: electrical power.

Because of a previous issue related to isolated power, Dillard had already worked up a room diagram using Microsoft Paint and Microsoft Word to identify every electrical outlet in each operating room and the corresponding breakers associated with the receptacles. This gave us a room-mapping diagram that proved to be very useful. We knew which breakers went where and we knew how much amp draw each receptacle could tolerate.
Practice Makes Perfect
Two dry runs took place the week before the surgery. An estimated 40 to 50 people were expected to have at least some involvement in the surgery, and everyone was there for the simulations. Of special interest was the custom-made, $100,000 operating bed donated by Kinetic Concepts Inc (KCI) of San Antonio, Tex. How would it be placed in relation to the anesthesia machines? Where would we locate the stereotactic guidance system? Where would everyone stand? Do we still have enough room to get a C-arm in the room?
After the room was set up for the first dry run, Dillard and Brainard identified every piece of equipment and each device’s corresponding electrical receptacle. Each electrical outlet was labeled for the equipment that was to be plugged into it. Dillard took the information and entered it into a spreadsheet to tally total amp draw for each receptacle. Several days later, the second dry run added new pieces of equipment to the room and forced us to make several equipment location changes.
In the end, the surgical teams had a room layout they could work comfortably in, and Dillard and Brainard had a power distribution model they were comfortable with. The stage was set for the actual surgery. My personal feelings were that our services had been appreciated and that this was when the biomed team would say, “Good-bye, have a nice case.” Not this time.
The entire OR team, including the surgeons and anesthesiologists, wanted the biomed team to remain throughout the case. They assured us that they were not about to unplug anything, move anything, or bring any equipment into the room without the prior approval of the biomed team. “After more than a year of negotiating the scientific and technical hazards of the case, the surgical team could not have plans jeopardized by a fried breaker,” the Dallas Morning News reported in its coverage of the surgery. We could not have said it better.

At the Ready
On the morning of Saturday, October 11, staff began to gather in the surgery department lounge. Surgeons, anesthesiologists, nurses, scrub techs, and biomeds all waited patiently for the call. The OR manager/team coordinator began checking with her groups: “Biomed, are you ready? Anesthesia, are you ready?” Everyone was, and, at 8:45 am, the twins were on their way to the operating room. At this point, Bill Picot, biomed team leader for critical-care services joined Dillard and Brainard for shift rotation and to provide additional support.

First the boys were placed on the KCI operating table, which was built specifically for this surgery and consisted of a unique frame design that allowed each boy to be secured in his own personal “clamshell.” The clamshells were actually two separate tables connected by a center lock. Each clamshell could be rotated 360 degrees independently while still connected to the other. When the time came, the sections could be pulled apart, making two separate operating tables that could not only rotate but also tilt.
While nurses and OR technicians prepared the boys, the neurosurgeons and craniofacial surgeons were concentrating on their responsibilities. Over the past year it had been a common sight to see the neurosurgeons holding and studying a three-dimensional model of the conjoined brains, intensely studying the tangled web of vessels interconnecting the two. Having seen and held the model myself, I gained a whole new respect for the skilled hands of these neurosurgeons. I saw no way that anyone could unravel that vascular bird’s nest without creating a blood bath.
Oh, What a Tangle
Shortly after 6:00 pm, the boys were snug in their clamshells fitted with SpongeBob SquarePants sheets and were ready for the craniofacial team. They began by removing the skin expanders that had been inserted under the boys’ scalps months in advance. Then they gently laid back the skin, exposing the skull. The neurosurgical team opened a section of the skull, exposing the brain. Before them was the entanglement of vessels that they had been studying for the past year. Cautiously they worked well into the night: clamp a vessel, snip it, seal it, and move on to the next. Clamp, snip, seal, move on. Then, at approximately 3:00 am, it happened.
Brainard to the Rescue
“Get biomed, we have a problem with the Bovie!” When the room had been set up, some of the electrosurgical units were placed under the operating table to allow for more working room around the table. This had concerned us from the beginning, mostly because of fluids, but also because of the possibility of having to remove a failed device. Either situation was not one we favored.
Dillard, now sleeping, had left Brainard in charge. She worked her way as close to the table as she possibly could without violating the sterile field. She needed to get a look at the Valley Lab Force FX generator. She could see that it was displaying an error code, and, having just returned from Valley Lab Service School the previous week, she quickly determined that the unit was overheating. Upon closer examination, she found that a portion of the drape had blocked the cooling fan. The drape was moved, the unit cooled down, the error code went away, and surgery continued uninterrupted.
We Have Two Boys
Around 11:00 am, the surgeons were satisfied that they had separated the final vessels connecting the boys. This was it! The OR was a buzz of activity. Everybody wanted to be involved in the actual separation. Everyone wanted to witness what they had all been working so hard to accomplish.

The KCI engineers were called into the room to loosen the connecting rod that held the two bed halves together. As the operating-room floor began to be visible between the boys and the last few vessels snipped and sealed, the boys were finally separate. At approximately 11:15 am, on October 12, Ahmed and Mohamed Ibrahim began living separate lives. Their vital signs remained strong and steady as the surgical team separated into two teams to work on each boy. The neurosurgeons’ jobs were done; they had just performed one of the most delicate surgical procedures ever undertaken. The craniofacial teams began the delicate process of covering the exposed craniums and closing the wounds created by the surgery. The services of the biomed team would not be needed beyond this point.

A Winning Team
Dillard, Brainard, and Picot did not leave their posts until both boys were transported from surgery to their beds in the ICU 34 hours after the separation surgery began. As representatives of the biomedical engineering department at Children’s Medical Center Dallas, they make me very proud. We had a small but very important part to play in this historical case, and I want to thank my team for their dedication. The exceptional job they do every day is highlighted at a time like this, but then this really was just another “day in the life” of a biomed at Children’s Medical Center Dallas.
An interesting “small world” fact is that Picot, Brainard, and Dillard are all from Killeen, Tex. Although she went to the same high school and lived within five miles of them, Brainard did not know Picot or Dillard. All three are graduates of the biomedical technology program at Texas State Technical College in Waco.
Ron Greenwalt has been an ARAMARK clinical technology services manager since 1992 and manager of biomedical services at Children’s Medical Center Dallas since June 2000.
Correction
In the December issue, the caption accompanying the photo on the top left-hand corner of page 33 should read: Author Lou Schonder, perfusionist Gankhuyag, and surgeon Dr. Bat-Undral.
The caption accompanying the photo on page 34 should read: We did it! POH volunteers Jim Burris and Lou Schonder pose with Dr. Bat-Undral and Shastin engineers after installing the oxygen manifold system donated by Denver’s Mile High Rotary Club.