|
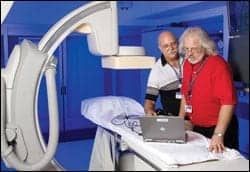
| Left to right, Richard Edwards, PACS specialist; and Paul Sherman, CCE, senior biomedical engineer, VA Center for Engineering & Occupational Safety and Health, St Louis. |
Americans have a long history of taking care of their soldiers, dating back to the 1636 law that dictated that disabled soldiers would be supported by the colony. Even with such roots, many people most strongly associate President Abraham Lincoln with the system that would become today’s Veterans Health Administration facilities, which is run by the US Department of Veterans Affairs.
Concluding his second inaugural address, Lincoln stated, “With malice toward none; with charity for all; with firmness in the right, as God gives us to see the right; let us strive on to finish the work we are in; to bind up the nation’s wounds; to care for him who shall have borne the battle and for his widow, and his orphan—to do all which may achieve and cherish a just and a lasting peace, among ourselves, and with all nations.”
As a result, many state-sponsored veterans homes were established. When the United States entered World War I in 1917, Congress established a new system of veterans’ benefits, with substantially more services added as a result of the Second World War. Since that time, the responsibilities and benefits dispensed through the VA expanded to create the most comprehensive system of assistance for veterans of any nation in the world.
The VA runs the largest integrated health care system in the United States. Its roughly 14,800 physicians and 61,000 nurses staff more than 1,000 hospitals, clinics, and nursing homes, providing a wide range of medical, surgical, and rehabilitative services to the 5.3 million veterans and their dependents who make up the patient base.
Among those teams are the 101 biomedical engineers and clinical engineers who work alongside about 850 technicians tending to more than 750,000 pieces of medical equipment valued at just over $4 billion.
“We have 157 hospitals in 21 networks, which include 51,000 inpatient beds, 862 clinics, and 134 nursing homes,” says Paul Sherman, CCE, senior biomedical engineer at the VA Center for Engineering & Occupational Safety and Health (CEOSH) in St Louis. Sherman’s office serves as a national support office for all of the VA’s hospitals. “I function as an in-house consultant for the VA on medical technology. I am also responsible for all hazard alerts and recalls on all medical equipment.”
In his role, Sherman is indicative of the VA’s successful approach to managing its vast territory. The organization provides autonomy to individual hospitals so they can operate efficiently given the specifics of their region, while simultaneously providing the support necessary to resolve any issues that may arise.
“If there are projects or concerns taking place that will impact all the hospitals, or a large percentage of them, rather than have each hospital try and handle it individually, I get involved at a national level and help to address the issue,” Sherman says. “And if a hospital has a specific problem, I function as a sounding board or a resource for them, to help enable them to solve their problems locally.”
This distinctive blend of local and national seems to strike the right balance for those in the field.
“There is definitely a sense of what you see at some of the largest hospital systems, but even more so here,” says Paul Canaris, who has worked for the VA for 31 years and is chief of biomedical engineering in Temple, Tex, which also includes the Waco and Austin locations. “Though we have hundreds of unique locations, we’re tied together from a community standpoint. We have common forums we can access to discuss day-to-day business; we also have commonality from the standpoint that we have one central office in Washington, DC, and the leadership coming out of there.”
Joining Forces
For about a decade, that community approach has been quite literal for the VA installations. There are 21 regional Veterans Integrated Service Networks (VISNs). These networks make it possible for regional neighbors to combine efforts.
 |
| Left to right, Marty Brunworth, biomedical engineering intern; Paul Sherman; and John A. Waldmann, biomedical engineering technician. |
At this time, only three of the VISNs (commonly pronounced “visions”) have an assigned biomedical engineer at the network level. Facilities in VISNs without a network-level biomedical engineer maintain that support at the hospital level.
“The facilities in VISN1 are separate VAs, but what we’ve done is create a consolidated program of clinical engineering for the region,” says Hank Stankiewicz, clinical engineer manager for VA New England, Bedford, Mass. Stankiewicz’s VISN, or VISN1, includes almost a dozen campuses throughout Maine, Vermont, New Hampshire, Massachusetts, Connecticut, and Rhode Island. “We set up this combined clinical engineering program so we can unify our efforts. We say that we are an outsource program, but we are in-house people.”
Within each VISN, specialties are assigned by location. In New England, for example, when robotic surgery came onto the scene, the VISN purchased systems for installation in its large tertiary systems in Connecticut and Boston. Today, as bariatric surgeries grow in numbers, an analysis is under way to determine which locations have the physical space and technical know-how to best support the technology.
“In other cases, it’s rather straightforward,” Stankiewicz says. When the VA made a big push for public-access defibrillators, members from the cardiac arrest committees, cardiology group, and emergency care teams worked together to determine what was best for the VISN. “We looked at it from a systemwide perspective and decided together what would serve us best for public access to fibrillation,” he says.
This is often the approach to common-use devices, so that regardless of the location—whether a physician is in a clinic or in the hospital—the machine will be the same. This is especially important within a VISN, as many clinicians rotate among VAs.
This unified effort is not without its difficulties. For VISN1, part of the challenge is not only managing services across a network of hospitals and clinics, but explaining to medical personnel that the problem may be presenting itself in one location, but that the cause is located hundreds of miles away.
“We have some integrated systems that cross campus lines, so it can become quite challenging with networked medical equipment, where the server may not be on the same site you are working in,” Stankiewicz explains. The soon-to-be-installed PACS server in VISN1, for instance, is going to be physically located in Boston, from where it will serve the entire network. “So if they experience a problem up in Manchester (NH), the cause may actually be down in Boston.”
This presents a distinct challenge for biomeds, who must look beyond simply servicing a broken piece of equipment.
“If something like an ECG machine breaks, you have to look at the ECG machine; then you have to look at the computer at your local facility, but the problem may actually be at the facility that is down at the Providence (RI) VA,” Stankiewicz says. “When a clinician in Maine comes to the biomedical tech and says, ‘I can’t read a film, what’s wrong?’ the clinician doesn’t want to hear that they have a power glitch down at the VA in Connecticut. So for a service guy, that’s a big paradigm shift; it’s a different mind-set.”
Even with its hurdles, the benefits of this collaborative effort far outweigh its negatives, according to Stankiewicz. One such positive is the increased ability to monitor patient safety.
“We have a very good national hazard recall and hazard notification system in place,” he says. The medical centers work closely with the VA’s National Center for Patient Safety (NCPS), as well as many other national groups, to ensure that the equipment is reliable and safe. Individual medical centers within the VISN also meet regularly to discuss safety issues. “Just recently, we were discussing a problem one of the nursing units was having with their infusion pumps,” Stankiewicz says. “We promptly examined it to determine if it was a unique situation or if it was a systemic problem.”
 |
| Richard Ivnik, chief biomedical engineer, left; and Paul Sherman troubleshoot the PACS monitors. |
Staying connected in this way means that when equipment malfunctions are discovered at one location, the biomedical team is able to target and rectify a minor patient safety issue before it becomes a major problem.
“If we realize that something has the potential to be a systemwide problem, there is a process in place which allows me to quickly notify headquarters and NCPS or the engineering service center, depending on what type of issue it is,” Stankiewicz says. “The beauty of it is that we can really solve a problem before it injures anybody. And I’m a big believer that if you really study the near misses, you can really solve a lot of problems without waiting for a disaster to occur.”
Aside from the NCPS, the individual VA locations have access to a broad base of support from inside the VA itself, according to Stankiewicz: the DC-based headquarter group, the CEOSH (of which Sherman is the head), and the Engineering Training Center in Little Rock, Ark.
He notes, “Being part of the VA gives me an advantage. I’m not working as an isolated clinical engineer. I have four different groups to help me do my job, and it is nice to be part of that structure.”
Staying in Touch
The focus on patient safety extends to the VA’s Biomedical Engineering Advisory Board (BEAB). Established about 4 years ago, the BEAB is made up of a group of field engineers and technicians who provide input from the local centers to management at the VA’s national headquarters.
“The BEAB provides the field perspective to headquarters,” Sherman, who is part of that team, says. “We have a number of topics we’ve identified to work on, and we’ve put together work groups to gather information about the issues.”
Pulling input from across all locations also serves to provide further commonality and structure to the medical centers.
“It allows us to address issues on more of a national level, so you don’t have to fight the same battles locally and reinvent the wheel a hundred times over,” says Canaris, who sits on the board as well. “This way we can take on issues, set up focus groups, and take the necessary steps to set policy and guidance for the entire system. It’s a big benefit when you have that kind of power working for you; you’re not solo on everything.”
This type of backing has become particularly valuable as the VA facilities, like the rest of the medical community, wrestle with rapidly changing technology and the real-world impact it has on patient data security issues and overall confidentiality. Members of the BEAB also address personnel issues for biomedical staff.
“Right now, we are looking at the grade structure for our technicians, nationwide,” says Stankiewicz, who is part of the board. “We are working to determine the best way to properly benchmark the biomed programs. We are also looking at standardization of customer-satisfaction surveys.”
Other national initiatives being addressed through the BEAB include how medical centers computerize patient records, as well as establishing medical equipment managing plans that are similar across networks, to simplify The Joint Commission inspection process.
Watching the Bottom Line
Being organized into VISNs also provides the VA centers with some additional muscle in negotiating contracts or purchasing new equipment.
“The government has a lot of contracts, but if you cross the eight territories like VISN1 does, companies are able to give an even better price than they would even on the government rate,” says Stankiewicz, whose VISN includes 11 individual campuses.
Also with an eye to being as fiscally conservative as possible, the VA has performed a biomedical equipment resource survey (BERS) each year for the past quarter-century. The BERS survey is both a local and a national measure of the efficiency of the organization’s biomedical programs.
BERS conducts a series of mathematical calculations and paradigms that allow for comparisons to be made locally, regionally, and nationally, as well as with a “7×7 matrix.”
“In a 7×7 matrix, a hospital like mine is compared to the next seven hospitals with a slightly higher inventory than mine and the next seven which are slightly lower,” Canaris says.
Information from the BERS survey makes it possible for an individual medical center to measure its total funding, staffing, resource usage, and number of contracts—among other factors—against similar facilities within the system.
 |
| Paul Sherman (standing), and left to right VA biomedical engineering technicians John A. Waldmann, and Derek Carr. |
“The data is then shared nationally, so you actually see how another hospital somewhere else in the country is doing,” Canaris says. “You are really able to see, as a program, how efficient you are, relative to the size of your facility. It’s a good tool for staffing and planning, obtaining resources, and determining if you’re heading in the right direction.”
Providing Top Care
Saving money where possible does not mean scrimping on patient care. In fact, many technological innovations, such as the standard use of bar coding, got their start in the VA hospitals. In keeping with that tradition, the medical centers continue to install and implement the latest standard of care.
“As biomeds, we are very heavily involved in life-cycle cost analysis and the selection of manufacturers when we purchase equipment, both in determining modality appropriateness and in maintaining state-of-the-art capabilities,” Canaris says.
Part of that role includes reviewing statistics about aging equipment and analyzing breakdown rates. When the recommendation is made to replace or add equipment, the VA biomeds are involved with that process as well. Canaris’ team recently oversaw the purchase and installation of a number of imaging modalities. “It was getting to the point where we were getting simultaneous, multiple failures on single units, which is not good,” he says. In less than 2 years, his region has replaced all patient monitors and installed PET cameras. “We are in the process of installing three new CTs—a 64-slice and two 16-slice systems—and a 3T MRI. Next, we’re going to upgrade our PACS systems and the patient charting system.”
Advancements happen at the nationwide level as well. “Right now I’m working with a group from our CIO’s office on a project to upgrade and install wireless networking in all the hospitals,” says Sherman, who also manages the financial benchmarking program for the VA. “It’s a huge project, and they wanted biomedical engineering’s input on it.” Sherman is also involved in providing guidance for an RFID pilot program at one of the hospitals at Minneapolis. “In addition, we have a satellite broadcast system and the studio is actually here in St Louis, so I’ve been able to bring people in to help provide training when appropriate,” he says. “One of the other things we’re also trying to implement at the moment is a wireless management program, not just for telemetry or for the wireless LAN, but across the board.”
This type of approach helps the VA fulfill its commitment and the commitment of the country—to care for those who have worn the nation’s uniform.
“Each VISN is designed to act as an integrated delivery system, tracking each of its veterans in the area,” Stankiewicz says. “We are committed to providing preventive medicine and caring for the veteran in his or her total health care issues.”
Dana Hinesly is a contributing writer for 24×7. For more information, contact .